Masks
There is still little to no scientific evidence for the effectiveness of cloth face masks in the general population in 2020. The introduction of mandatory masks couldn’t contain or slow the epidemic in most countries. If used improperly, masks may even increase the risk of infection. Not a single research study advocated for masks before 2020. All stated that they are at best ineffective and might even be harmful to our health.
January 2021
Facemasks in the COVID-19 era: A health hypothesis
“The existing scientific evidences challenge the safety and efficacy of wearing facemask as preventive intervention for COVID-19. The data suggest that both medical and non-medical facemasks are ineffective to block human-to-human transmission of viral and infectious disease such SARS-CoV-2 and COVID-19, supporting against the usage of facemasks. Wearing facemasks has been demonstrated to have substantial adverse physiological and psychological effects. These include hypoxia, hypercapnia, shortness of breath, increased acidity and toxicity, activation of fear and stress response, rise in stress hormones, immunosuppression, fatigue, headaches, decline in cognitive performance, predisposition for viral and infectious illnesses, chronic stress, anxiety and depression. Long-term consequences of wearing facemask can cause health deterioration, developing and progression of chronic diseases and premature death. Governments, policy makers and health organizations should utilize prosper and scientific evidence-based approach with respect to wearing facemasks, when the latter is considered as preventive intervention for public health.”
https://www.sciencedirect.com/science/article/pii/S0306987720333028
December 1, 2020
Even the updated document from WHO “Mask use in the context of COVID-19” Interim Guidance, dated December 1, 2020 states the following on Page 8:
“At present there is only limited and inconsistent scientific evidence to support the effectiveness of masking of healthy people in the community to prevent infection with respiratory viruses, including SARS-CoV-2.”
“A large randomized community-based trial in which 4862 healthy participants were divided into a group wearing medical/surgical masks and a control group found no difference in infection with SARS-CoV-2 (76). A recent systematic review found nine trials (of which eight were cluster-randomized controlled trials in which clusters of people, versus individuals, were randomized) comparing medical/surgical masks versus no masks to prevent the spread of viral respiratory illness. Two trials were with healthcare workers and seven in the community. The review concluded that wearing a mask may make little or no difference to the prevention of influenza-like illness (ILI) (RR 0.99, 95%CI 0.82 to 1.18) or laboratory confirmed illness (LCI) (RR 0.91, 95%CI 0.66-1.26)”
Page 10:
“The potential disadvantages of mask use by healthy people in the general public include:
• headache and/or breathing difficulties, depending on type of mask used (55);
• development of facial skin lesions, irritant dermatitis or worsening acne, when used frequently for long hours (58, 59, 127);
• difficulty with communicating clearly, especially for persons who are deaf or have poor hearing or use lip reading (128, 129);
• discomfort (44, 55, 59)
• a false sense of security leading to potentially lower adherence to other critical preventive measures such as physical distancing and hand hygiene (105);
• poor compliance with mask wearing, in particular by young children (111, 130-132);
• waste management issues; improper mask disposal leading to increased litter in public places and environmental hazards (133);
• disadvantages for or difficulty wearing masks, especially for children, developmentally challenged persons, those with mental illness, persons with cognitive impairment, those with asthma or chronic respiratory or breathing problems, those who have had facial trauma or recent oral maxillofacial surgery and those living in hot and humid environments”
https://www.who.int/publications/i/item/advice-on-the-use-of-masks-in-the-community-during-home-care-and-in-healthcare-settings-in-the-context-of-the-novel-coronavirus-(2019-ncov)-outbreak
November 2, 2020
An Evidence Based Scientific Analysis of Why Masks are Ineffective, Unnecessary, and Harmful
By Jim Meehan, MD
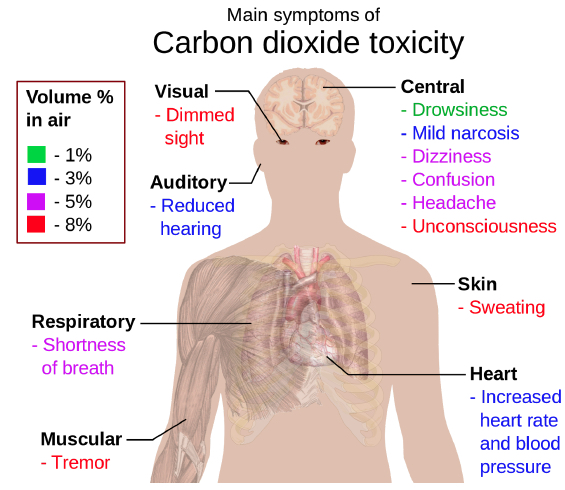
“Masks trap CO2 rich respiratory exhalations at the mask-mouth interface, force re-breathing of CO2 rich exhalations, raise carbon dioxide blood (CO 2 ) levels.”
“Face masks trap exhaled viral particles in the mouth/mask interspace. The trapped viral particles are prevented from removal from the airways. The mask wearer is then forced to re-breathe the viral particles, thus increasing infectious viral particles in the airways and lungs.”
“By wearing a mask, the exhaled viruses will not be able to escape and will concentrate in the nasal passages, enter the olfactory nerves and travel into the brain.”
Masks and blood supply to the brain of children
October, 2020
Masks cause Oxygen deprivation and permanent neurological damage, especially in the developing brains of children.
Dr. Margarite Griesz-Brisson MD, PhD, Neurologist and Neurophysiologist with a PhD in Pharmacology, with special interest in neurotoxicology, environmental medicine, neuroregeneration and neuroplasticity.
August 13, 2020
Carl Heneghan on Masks – clinical epidemiologist with expertise in evidence-based medicine, research methods, and evidence synthesis.
He is Director of the NIHR SPCR Evidence Synthesis Working Group a collaboration of nine primary care departments across UK universities. He set up and directs the Oxford COVID Evidence Service, has over 400 peer-reviewed publications; published 95 systematic reviews. He is Editor in Chief of BMJ Evidence-Based Medicine, and Editor of the Catalogue of Bias.
July 2020
Masks are neither effective nor safe:
A summary of the science
Page 1:
“In this meta-analysis, face masks were found to have no detectable effect against transmission of viral infections. (1) It found: “Compared to no masks, there was no reduction of influenza-like illness cases or influenza for masks in the general population, nor in healthcare workers.”
Page 3:
“Surgical mask wearers had significantly increased dyspnea after a 6-minute walk than non-mask wearers.”
“Researchers are concerned about possible burden of facemasks during physical activity on pulmonary, circulatory and immune systems, due to oxygen reduction and air trapping reducing substantial carbon dioxide exchange. As a result of hypercapnia, there may be cardiac overload, renal overload, and a shift to metabolic acidosis”
Page 3
Risks of cloth masks
“Healthcare workers wearing cloth masks had significantly higher rates of influenza-like illness after four weeks of continuous on-the-job use, when compared to controls.
The increased rate of infection in mask-wearers may be due to a weakening of immune function during mask use. Surgeons have been found to have lower oxygen saturation after surgeries even as short as 30 minutes. (40) Low oxygen induces hypoxia-inducible factor 1 alpha (HIF-1). (41) This in turn down-regulates CD4+ T-cells. CD4+ T-cells, in turn, are necessary for viral immunity.”
https://www.primarydoctor.org/masks-not-effect
May 2020
CDC
Nonpharmaceutical Measures for Pandemic Influenza in Nonhealthcare Settings—Personal Protective and Environmental Measures
Page 4
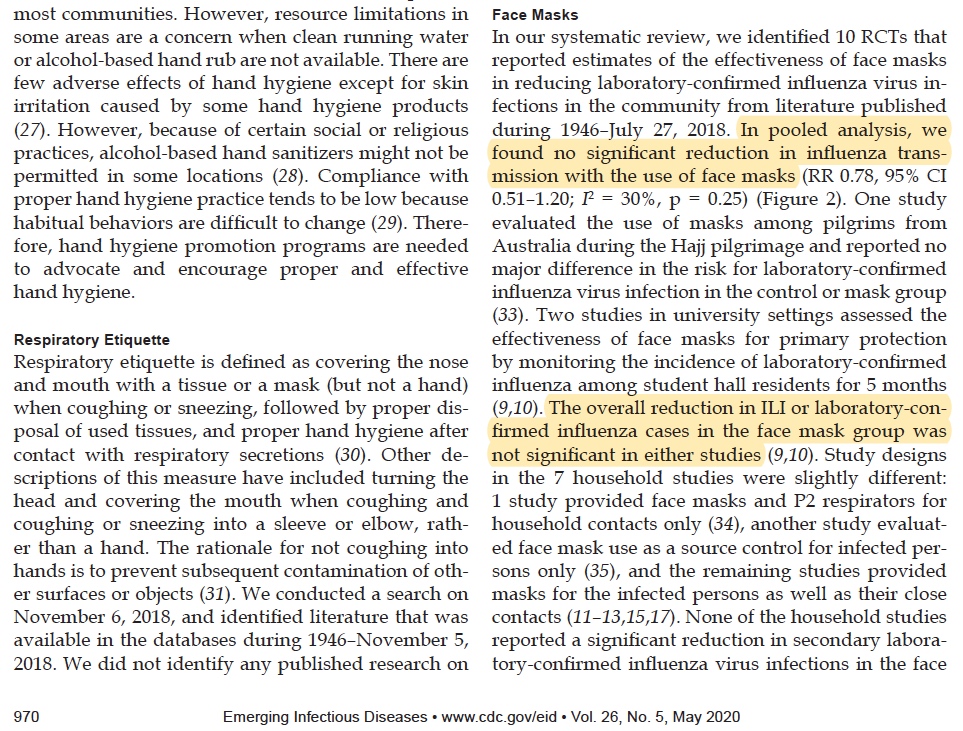
“In pooled analysis, we found no significant reduction in influenza transmission with the use of face masks”
“The overall reduction in ILI or laboratory-confirmed influenza cases in the face mask group was not significant in either studies”.
Page 5
“There is limited evidence for their effectiveness in preventing influenza virus transmission either when worn by the infected person for source control or when worn by uninfected persons to reduce exposure. Our systematic review found no significant effect of face masks on transmission of laboratoryconfirmed influenza.”
https://wwwnc.cdc.gov/eid/article/26/5/19-0994_article
Mai, 21, 2020
Universal Masking in Hospitals in the Covid-19 Era
“We know that wearing a mask outside health care facilities offers little, if any, protection from infection.”
https://www.nejm.org/doi/full/10.1056/NEJMp2006372.
April 6, 2020
Masks are neither effective nor safe:
World Health Organization WHO – Advice on the use of masks in the context of COVID-19
Page 1:
“Studies of influenza, influenza-like illness, and human coronaviruses provide evidence that the use of a medical mask can prevent the spread of infectious droplets from an infected person to someone else and potential contamination of the environment by these droplets. There is limited evidence that wearing a medical mask by healthy individuals in the households or among contacts of a sick patient, or among attendees of mass gatherings may be beneficial as a preventive measure.
However, there is currently no evidence that wearing a mask (whether medical or other types) by healthy persons in the wider community setting, including universal community masking, can prevent them from infection with respiratory viruses, including COVID-19.”
Page 2:
“Persons with symptoms should:
• wear a medical mask, self-isolate, and seek medical advice All persons should:
• avoid groups of people…… says NOTHING about the general and healthy population wearing masks!
Continuing on Page 2:
“However, the following potential risks should be carefully taken into account in any decision-making process:
• self-contamination that can occur by touching and reusing contaminated mask
• depending on type of mask used, potential breathing difficulties”
https://apps.who.int/iris/bitstream/handle/10665/331693/WHO-2019-nCov-IPC_Masks- 2020.3-eng.pdf?sequence=1&isAllowed=y
April 1, 2020
Michael Klompas, M.D., M.P.H., et. al., Universal Masking in Hospitals in the Covid-19 Era , New England Journal of Medicine, N Engl J Med
“We know that wearing a mask outside health care facilities offers little, if any, protection from infection.”
“It is also clear that masks serve symbolic roles. Masks are not only tools, they are also talismans that may help increase health care workers’ perceived sense of safety, well-being, and trust in their hospitals. Although such reactions may not be strictly logical, we are all subject to fear and anxiety, especially during times of crisis. One might argue that fear and anxiety are better countered with data and education than with a marginally beneficial mask.”
https://www.nejm.org/doi/full/10.1056/NEJMp2006372
June 3, 2019
Contamination by respiratory viruses on outer surface of medical masks used by hospital healthcare workers
“Respiratory pathogens on the outer surface of the used medical masks may result in self-contamination”.
https://pubmed.ncbi.nlm.nih.gov/31159777/
June, 2, 2018
Surgical masks as source of bacterial contamination during operative procedures
“The source of bacterial contamination in surgical masks was the body surface of the surgeons rather than the operating room environment”.
https://pubmed.ncbi.nlm.nih.gov/30035033/
August 2016
Canadian Centre for Occupational Health and Safety:
“The filter material of surgical masks does not retain or filter out submicron particles;
Surgical masks are not designed to eliminate air leakage around the edges;
Surgical masks do not protect the wearer from inhaling small particles that can remain airborne for long periods of time.”
“Between 2004 and 2016 at least a dozen research or review articles have been published on the inadequacies of face masks. All agree that the poor facial fit and limited filtration characteristics of face masks make them unable to prevent the wearer inhaling airborne particles.”
2015
A cluster randomised trial of cloth masks compared with medical masks in healthcare workers
“This study is the first RCT of cloth masks, and the results caution against the use of cloth masks. This is an important finding to inform occupational health and safety. Moisture retention, reuse of cloth masks and poor filtration may result in increased risk of infection. Penetration of cloth masks by particles was almost 97% .”
https://bmjopen.bmj.com/content/5/4/e006577
2015
Da Zhou et al., reviewing the literature in 2015, concluded that “there is a lack of substantial evidence to support claims that facemasks protect either patient or surgeon from infectious contamination.”
https://journals.sagepub.com/doi/pdf/10.1177/0141076815583167
2014
Carøe, in a 2014 review based on four studies and 6,006 patients, wrote that “none of the four studies found a difference in the number of post-operative infections whether you used a surgical mask or not.”
https://europepmc.org/article/med/25294675
2014
Salassa and Swiontkowski, in 2014, investigated the necessity of scrubs, masks and head coverings in the operating room and concluded that “there is no evidence that these measures reduce the prevalence of surgical site infection.”
https://journals.lww.com/jbjsjournal/Abstract/2014/09030/Surgical_Attire_and_the_Operating_Room__Role_in.11.aspx
2014
Lipp and Edwards reviewed the surgical literature in 2014 and found “no statistically significant difference in infection rates between the masked and unmasked group in any of the trials.” Vincent and Edwards updated this review in 2016 and the conclusion was the same.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD002929.pub2/full
2010
Surgeons at the Karolinska Institute in Sweden, recognizing the lack of evidence supporting the use of masks, ceased requiring them in 2010 for anesthesiologists and other non-scrubbed personnel in the operating room. “Our decision to no longer require routine surgical masks for personnel not scrubbed for surgery is a departure from common practice. But the evidence to support this practice does not exist,” wrote Dr. Eva Sellden.
https://pubs.asahq.org/anesthesiology/article/113/6/1447/9572/Is-Routine-Use-of-a-Face-Mask-Necessary-in-the
2010
Webster et al., in 2010, reported on obstetric, gynecological, general, orthopaedic, breast and urological surgeries performed on 827 patients. All non-scrubbed staff wore masks in half the surgeries, and none of the non-scrubbed staff wore masks in half the surgeries. Surgical site infections occurred in 11.5% of the Mask group, and in only 9.0% of the No Mask group.
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1445-2197.2009.05200.x
2009
Zahid Mehmood Bahli did a systematic literature review in 2009 and found that “no significant difference in the incidence of postoperative wound infection was observed between masks groups and groups operated with no masks.”
https://pubmed.ncbi.nlm.nih.gov/20524498/
2001
Ana E. Figueiredo, et al., in 2001, reported that in five years of doing peritoneal dialysis without masks, rates of peritonitis in their unit were no different than rates in hospitals where masks were worn.
http://www.advancesinpd.com/adv01/21Figueiredo.htm
2001
A review by M.W.Skinner and B.A.Sutton in 2001 concluded that “The evidence for discontinuing the use of surgical face masks would appear to be stronger than the evidence available to support their continued use.”
https://journals.sagepub.com/doi/pdf/10.1177/0310057X0102900402
2001
Lahme et al., in 2001, wrote that “surgical face masks worn by patients during regional anaesthesia, did not reduce the concentration of airborne bacteria over the operation field in our study. Thus they are dispensable.”
https://europepmc.org/article/med/11760479
1991
In Tunevall’s 1991 study, a general surgical team wore no masks in half of their surgeries for two years. After 1,537 operations performed with masks, the wound infection rate was 4.7%, while after 1,551 operations performed without masks, the wound infection rate was only 3.5%.
https://link.springer.com/article/10.1007/BF01658736
1989
Laslett and Sabin, in 1989, found that caps and masks were not necessary during cardiac catheterization. “No infections were found in any patient, regardless of whether a cap or mask was used,” they wrote.
https://onlinelibrary.wiley.com/doi/abs/10.1002/ccd.1810170306
Sjøl and Kelbaek came to the same conclusion in 2002.
https://europepmc.org/article/med/11924291
1980
Ha’eri and Wiley, in 1980, applied human albumin microspheres to the interior of surgical masks in 20 operations. At the end of each operation, wound washings were examined under the microscope. “Particle contamination of the wound was demonstrated in all experiments.”
https://europepmc.org/article/med/7379387
1975
Ritter et al., in 1975, found that “the wearing of a surgical face mask had no effect upon the overall operating room environmental contamination.”
https://pubmed.ncbi.nlm.nih.gov/1157412/
We urgently need your support !!
There are many easy ways how to do this. Please find the information here:
>How to Support Us <
>Shop at our Affiliate Partner Shops<
Find books, nutritions, vitamins, groceries, outdoor products, travel deals, and many more on our pages:
Dietary Supplements, Immune Support
or please Donate here 🙂
Mask debate in Charleston, SC City Council on August 17, 2021
Parents speak up during a City Council meeting in Charleston, SC on August 17, 2021
The City of Charleston planned to implement a mask mandate for daycare centers, public and private schools for all adults and children two years and older. During the City Council session, parents were allowed to speak up. The City of Charleston later failed to get the necessary votes for the mandate.
The end of the mask debate
Bringing the mask debate to an end with the knowledge of Natural Law and our immutable human rights.
Are Face Masks Effective? The Evidence.
Lots of evidence, informations and links to research studies.
https://swprs.org/face-masks-evidence/
In many states, coronavirus infections strongly increased after mask mandates had been introduced. The following charts show the typical examples of Austria, Belgium, France, Germany, Ireland, Italy, Spain, the UK, California, Hawaii and Texas.
What to say to store clerks and cops who try to violate your personal liberty and civil rights
https://static1.squarespace.com/static/5ec33703d876e52434d8b91c/t/5ffd3f23a4c138036b6e094d/1610432294703/FREE+GUIDE+-+No+Mask+No+Service+-+Peggy+Hall+The+Healthy+American.pdf
https://www.thehealthyamerican.org/masks-dont-work
All information is deemed accurate but not guaranteed and should be independently verified.